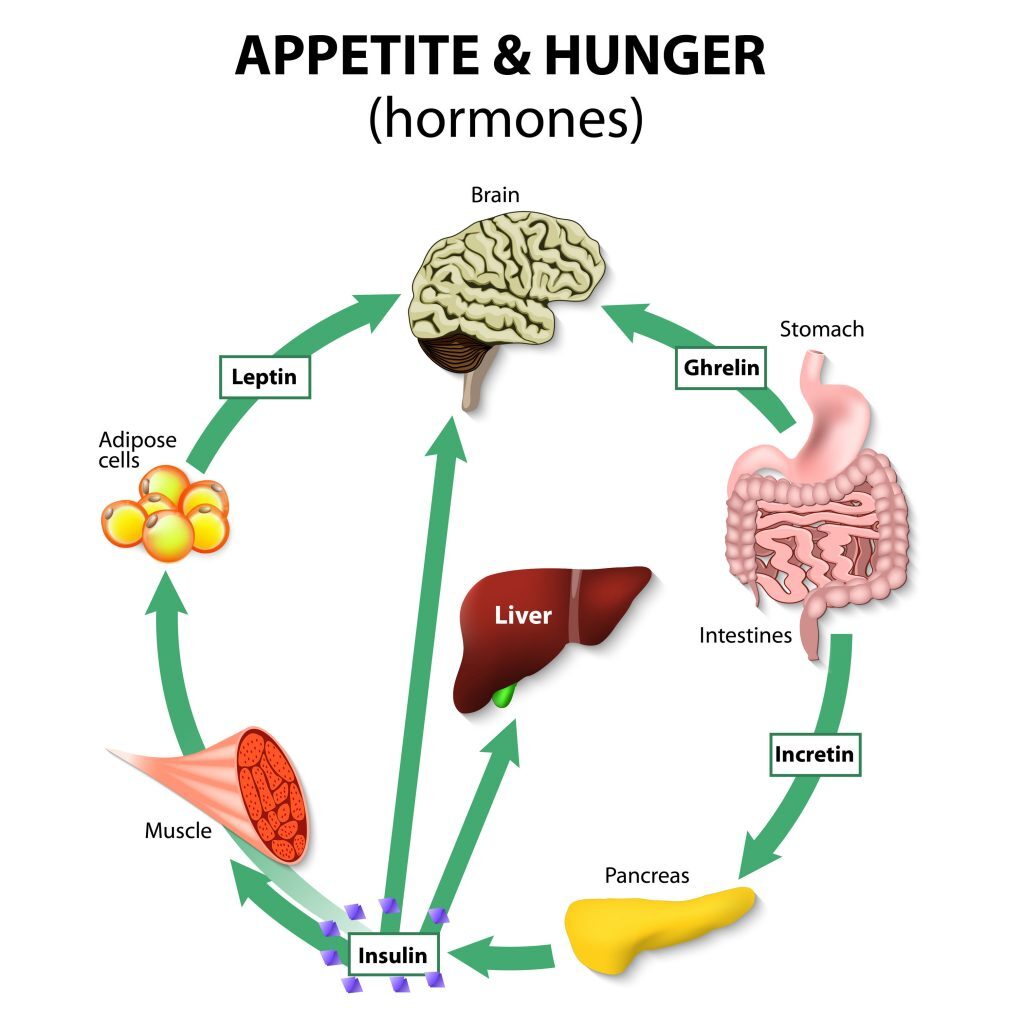
Appetite is the desire to eat food, felt as hunger. Appetite exists in all higher life-forms and serves to regulate adequate energy intake to maintain metabolic needs, regulated by a close interplay between the digestive tract, adipose tissue, and the hormones.
In stress, appetite levels increase and result in an increase in food intake. Dysregulation of appetite contributes to anorexia nervosa, bulimia nervosa, cachexia, overeating, and binge eating disorder.
The hypothalamus, a part of the brain, is the main regulatory organ for the human appetite. The neurons that regulate appetite appear to be mainly serotonergic. The hormones are sensed by eternal stimulus, which modify the hypothalamic response, produced by the digestive tract and adipose tissue (leptin and adiponectin).
Appetite regulated by a complex system of central and peripheral signals which interact to modulate the individual response to nutrient ingestion. Peripheral regulation includes
- Satiety signals
- Adiposity signals.
The central nervous system controls by several effectors like neuropeptidergic , monoaminergic, and endocannabinoid systems.
Which Hormones regulate Appetite?
Calcitonin
Released in response to gastrin and changes in serum calcium levels. Calcitonin secreted by the thyroid, GI tract, and pancreas. A complementary signal responsible for fine-tuning the eating process.
Amylin
a partner hormone to insulin, released after meals secreted by the pancreas. It slows the emptying of our stomach and suppresses glucagon (glucagon raises blood sugar)
GLP-1
GLP-1 breaks when blood glucose levels are elevated. It is secreted by cells in the gut in proportion to the amount of energy ingested Stimulates insulin and amylin secretion, may assist in signaling the brain to stop eating
Leptin
Released with low-calorie intake and low body fat levels. Secreted by fat cells Low leptin means a slower metabolism and drive to increase food consumption. Administering leptin analogs in humans is ineffective for appetite suppression. Leptin exists to prevent starvation, not to lose weight. leptin is provided along with amylin, slight fat loss may occur.
Gastrin
Protein dense foods are the most potent stimulator of gastrin. They secreted by cells in the stomach or small intestine initiates the digestion process.
Secretin
Secretin liberates when acids react with the small intestine by the cells and produces pancreatic fluid which inhibits gastrin and enhances the effects of cholecystokinin.
Cholecystokinin (CCK)
Cholecystokinin releases when protein and fat enter the small intestine and signal the pancreas to produce enzymes that inhibit gastrin and stimulates gallbladder contraction, and triggers satiety in the brain.
Gastric inhibitory polypeptide (GIP)
Gastric inhibitory polypeptide (GIP) releases when food enters the small intestine. It also enhances insulin release, inhibits gastric secretions and motility. Motilin releases when bicarbonate is dumped into the small intestine, when fasting promotes muscle contraction of GI tract or released between meals notice borborygmic (growling stomach).
Somatostatin
Somatostatin released between meals to reduce digestive activity, particularly, secreted by the stomach, intestine, and pancreas which Slows gastric emptying, reduces GI muscle contractions and blood flow to gut PYY 3- 36. They may be released in the hours following a meal, presumably to suppress appetite and secreted by the small or large intestine which Inhibits stomach motility while increasing water and electrolyte absorption in the colon and also suppress pancreatic enzyme secretion. Obesity seems to be a PYY 3-36 deficient state
Ghrelin
Ghrelin has various roles. It is also called the ‘hunger hormone’ because it enhances appetite, increases the absorption of food, and encourages the accumulation of fat. Ghrelin increases food consumption by up to 30 percent when given to humans.
Released in response to low food intake/fasting Secreted by cells of the stomach, pancreas, placenta, kidney, pituitary, and hypothalamus also Stimulates the release of growth hormone to encourage eating and acts to regulate energy balance.
However, Eating lowers levels of ghrelin. Various nutrients slow down the release of ghrelin to various degrees; carbohydrates and proteins reduce ghrelin development and release to a greater extent than fats.
Adiponectin
Adiponectin or adipocyte is a related protein is a 244-amino acid protein secreted from adipose tissue. The plasma concentration of adiponectin is also, reciprocally correlated with adiposity in humans. Studies show that treatment with adiponectin can reduce body weight gain, increase insulin sensitivity, and decrease lipid levels. thus adiponectin as well as increasing energy expenditure also provide protection against insulin resistance and atherogenesis.
Resistin
Resistin is produced by adipose tissue and appears to increase insulin resistance, Moreover, It is increased in obese people and falls after weight loss, resistin may contribute to the development of insulin resistance and diabetes in obesity, its role in the pathogenesis of obesity remains to be defined.
Pancreatic-appetite Hormones regulation
Insulin: insulin is the first adiposity signal to be described and leptin, is positively correlated with long-term energy balance. Moreover, Plasma insulin concentrations depend on peripheral insulin sensitivity, with visceral fat being a key determinant. leptin levels, which are relatively insensitive to acute food intake, insulin secretion increases rapidly after a meal. Insulin is an anabolic hormone and increases appetite.
Pancreatic polypeptide
Pancreatic polypeptide (PP) is a member of the PP-fold family of peptides which also includes peptide YY (PYY) and NPY. in addition, It is produced by cells of the islets of Langerhans, exocrine pancreas, and distal gastrointestinal tract. Plasma PP concentrations show diurnal variation, with the lowest levels in the early hours of the morning and highest in the evening. PP directly reduces appetite via the brain.
Oxyntomodulin
Oxyntomodulin released in proportion to calorie intake from the L cells of the small intestine. Central and peripheral OXM acutely reduce food intake. The action of GLP-1 and OXM on food intake may be mediated by the GLP-1 receptor. OXM reduces appetite by repression of ghrelin.
Central Regulators of Appetite
Hypothalamic neuronal pathways regulating appetite regardless of daily variation in food intake and energy expenditure, body weight remains stable over long periods of time. The hypothalamus is essential for the regulation of appetite and energy balance. The brain initiates responses to feeding even before the ingestion of food. The sight and smell of food stimulates exocrine and endocrine secretions in the gut as well as increasing gut motility. Ingestion of food stimulates mechanoreceptors leading to distension and propulsion to accommodate the food. As the food is drive through the gut regions of the intestines secrete various hormones that circulate to the brain and impact hypothalamic responses.
Hypothalamic Lipid Metabolism and Energy Homeostasis
Within the central nervous system, the metabolism of fatty acids is primarily for the purposes of membrane function and the central regulation of energy metabolism. As well as Fats do not serve as a major source of energy within the brain.
Serotonin
Serotonin (5-HT) is a widespread neurotransmitter that acts on a number of receptor subtypes found at high density in the limbic system as well as in the hypothalamus. 5-HT stimulates noradrenaline release and modifies behavior and mood. 5-HT shows the most consistent inhibition of food intake. Serotonin may directly influence the melanocortin pathway.
The dopaminergic system is integral to reward- induced feeding behavior. Other systems, such as those mediated by serotonin, may also be able to modulate both reward circuitry and homeostatic mechanisms controlling feeding. The noradrenergic system also plays a role in appetite regulation, with activation of α1- and β2- adrenergic receptors inhibiting food intake.
Zinc:
Leptin levels decrease in response to zinc depletion and increases after zinc supplementation. Particularly, the magnitude of leptin level changes were proportional to the changes of cellular zinc. Also, Zinc increases TNFa and IL-2 cytokine production; Adequate zinc levels reduce appetite, possibly by increasing brain sensitivity to leptin.
Probiotics:
Recently, a potential link between gut microbiota and obesity has emerged. The study by Cani et al., [2011] evaluated the effect of prebiotics on plasma levels of gut hormones in healthy subjects. Additionally, Prebiotic treatment reports that increased gut microbiota fermentation, decreased appetite, and improved postprandial glucose responses. Estrogen deficiency might result in a higher energy intake and increased body weight. Food intake varies across the menstrual cycle. Women tend to eat more in the luteal phase (the premenstrual period) compared with the follicular phase.
Testosterone
Testosterone has less effect on food intake, many people supplementing anabolic doses of testosterone (e.g. bodybuilders) do report increased appetite. Including a balanced intake of omega-6, omega-3 fats can help with appetite regulation. Comparatively, A high protein diet can reduce appetite. Fiber seems to help control appetite. Refined carbohydrates, appear to increase appetite.
Sources:
- De Silva, A., & Bloom, S. R. (2012). Gut hormones and appetite control: a focus on PYY and GLP-1 as therapeutic targets in obesity. Gut and liver, 6(1), 10.
- Marić, G., Gazibara, T., Zaletel, I., Labudović Borović, M., Tomanović, N., Ćirić, M., & Puškaš, N. (2014). The role of gut hormones in appetite regulation. Acta Physiologica Hungarica, 101(4), 395-407.
- Little, T. J., Russo, A., Meyer, J. H., Horowitz, M., Smyth, D. R., Bellon, M., … & Feinle–Bisset, C. (2007). Free fatty acids have more potent effects on gastric emptying, gut hormones, and appetite than triacylglycerides. Gastroenterology, 133(4), 1124-1131.



